Symptomatic Hemorrhoid Treatment
Rubber Band Ligation — Rubber band ligation is the most commonly used technique for the treatment of symptomatic bleeding internal hemorrhoids. This hemorrhoid treatment technique is effective, inexpensive, and easy to perform and only rarely causes serious complications.
Patients with grade II or III internal hemorrhoids are the best candidates for rubber band ligation. External tags and external hemorrhoids are not to be treated with this technique, as it would cause excruciating pain. Banding procedures are typically contraindicated in patients with coagulopathies and those on anticoagulation medications, and patients with cirrhosis and portal hypertension, because of the risk of significant delayed hemorrhage. In the authors’ experience, patients on aspirin therapy can safely undergo rubber band ligation, with a low risk of bleeding. Banding is relatively contraindicated in immunocompromised patients (eg, chemotherapy administration, HIV/AIDS) because of risks of infection and sepsis.
When performed by a properly trained physician or gastroenterologist , this procedure does not require any anesthesia (local or intravenous). Usually, only one hemorrhoidal column should be treated at a time to minimize excessive tissue necrosis. However, if the patient tolerates the procedure with only minimal discomfort, then several hemorrhoids can be banded during the same session. As many as three bands in a single column may be safely performed. If multiple sessions are needed, then repeat banding procedures can be performed in three- to four-week intervals to allow any swelling and ulcerations to subside. Many patients complain of anal or rectal “tightness” after the procedure.
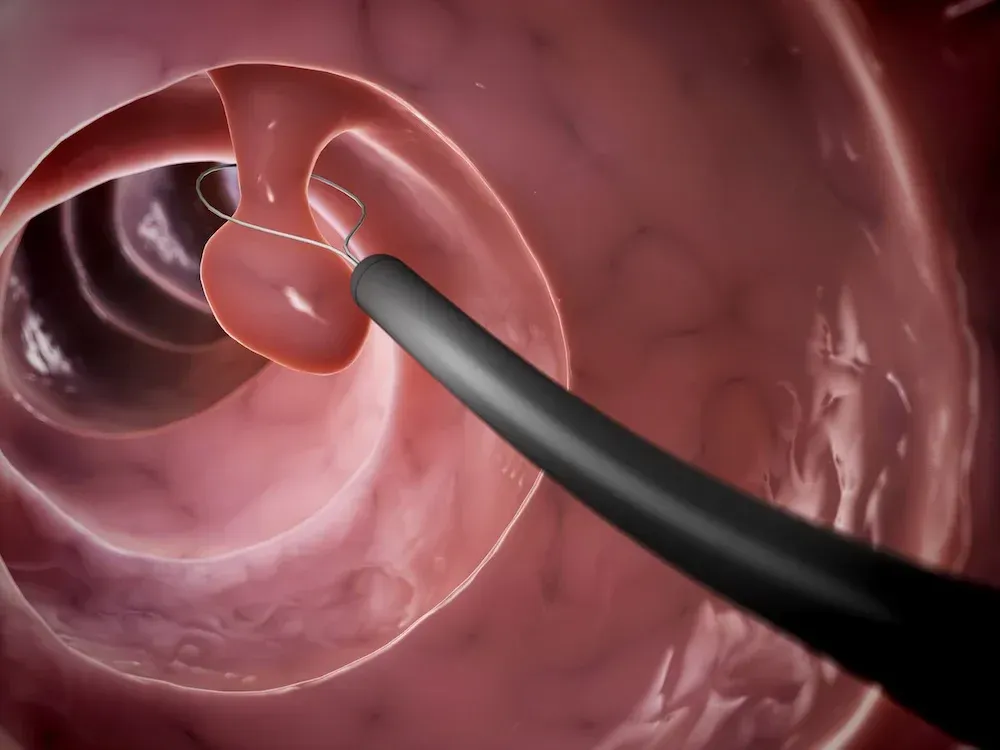
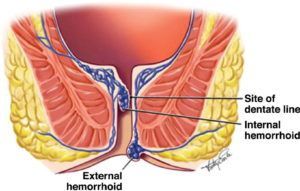
Patients are placed in the semi-inverted jackknife or left lateral position. The procedure is performed through the anoscope, and small rubber band rings are placed onto the internal hemorrhoids traditionally using a forceps, but other methods have been developed. When a forceps ligator is used to apply the bands, an assistant is required to stabilize the anoscope. Once the involved hemorrhoid is identified through an anoscope, the rubber ring ligating drum with two rubber rings is placed into the anal canal. The largest internal hemorrhoid should be treated first. The internal hemorrhoid is grasped with forceps, and the excess tissue is pulled toward the tip or drum of the handheld ligator gun apparatus while the trigger causes the release of the rubber band. The rubber rings are then advanced down to the neck of the hemorrhoid. The key technical point is to ensure the bands are placed at least 5 mm above the dentate line to avoid placement onto somatically innervated tissue. Severe pain will result from misapplication of the band below the dentate line or from associated spasm. Thus, prior to rubber band release, the patient should be questioned about the presence of pain, which may indicate the need to select a point more proximal in the anal canal. If a patient experiences intense or excruciating pain as the rubber band is placed, then the band should be removed immediately by cutting the rubber band.
Other application techniques have been described. Each uses the same principles as the traditional forceps approach described above.
- Endoscopic suction ligator – An alternative technique involves suction of the symptomatic hemorrhoid into the ligating drum, which is attached to an endoscope. The ring is deployed through a trigger passed through the biopsy channel of the endoscope. This approach may allow for adequate ligation with fewer treatment sessions. A single-handed nonendoscopic ligating device has also been used successfully and is less expensive than the endoscopic device.
- Wall suction ligator – Another technique uses a vacuum suction band ligator. The application of the rubber band using wall suction can be performed in fewer sessions compared with the standard forceps technique (1.2 versus 2 sessions). The principles are the same, but the rubber band ligator is attached to wall suction. The operator places the drum with the rubber band against the hemorrhoid. Suction pulls the hemorrhoid into the drum, and the rubber band is deployed. The technical advantage is that the operator can hold the ligator and apply the band with one hand and hold the anoscope with the other unassisted.
Successful ligation results in thrombosis of the hemorrhoid and the development of localized submucosal scarring. The banded hemorrhoidal tissues immediately become ischemic and then necrotic in the next three to five days, forming an ulcerated tissue bed. Complete healing occurs several weeks later.
One of the largest series to describe long-term outcomes of rubber band ligation included 805 patients who underwent 2114 ligations (median of two ligations in each patient). Excluding 104 patients who were lost to follow-up, treatment was considered successful in 71 percent (80 percent when considering patients who underwent repeated treatment after initial failure). Success rates were similar for all degrees of hemorrhoids. A higher failure rate was observed in patients who required placement of four or more bands.
In a meta-analysis of 12 trials, bleeding stopped after rubber band ligation in up to 90 percent of patients; 78 to 84 percent of those with grade III (prolapsing) hemorrhoids reported symptomatic improvement, and only 50 percent of patients with grade IV hemorrhoids had improvement. The most common complications are bleeding and pain (8 to 80 percent). However, the success rate often decreases with longer follow-up (eg, 40 to 50 percent at one year).
In a meta-analysis of 18 trials, rubber band ligation was more effective than injection sclerotherapy or infrared coagulation for the treatment of grade I, II, and III hemorrhoids, requiring fewer treatment sessions. The risk of complications and pain tended to be greater for rubber band ligation compared with other techniques. Compared with surgery, rubber band ligation had more recurrent symptoms but was associated with fewer complications and pain.
Following rubber band ligation, the most frequent complication is pain, which occurs in approximately 8 percent. Other complications include:
- Delayed hemorrhage – Delayed hemorrhage can occur when the rubber band dislodges, typically two to four days after application or with ulceration and mucosal sloughing, which can occur five to seven days after the procedure. Bleeding can be significant in patients with coagulation abnormalities.
- Hemorrhoidal thrombosis – Hemorrhoids distal to the treated hemorrhoid can thrombose, leading to pain or a palpable mass. ●Localized infection – Localized infection or abscess can occur at the site of band ligation. Persistent pain, fever, or foul-smelling rectal drainage may signal the onset of infection. Surgical drainage may be required.
- Sepsis – Fulminant sepsis after hemorrhoid ligation is rare but has been reported.
- Urinary retention.
The post Symptomatic Hemorrhoid Treatment appeared first on Gastro SB.