Hemorrhoid Banding
Rubber Band Ligation for Hemorrhoids
If you’ve ever had hemorrhoids, you know how uncomfortable, embarrassing or painful they can be. Hemorrhoids are very common in both men and women and, according to the Mayo Clinic, will affect almost three out of four adults in their lifetime. Many different factors can contribute to hemorrhoids forming, such as straining during bowel movements or not eating enough fiber.
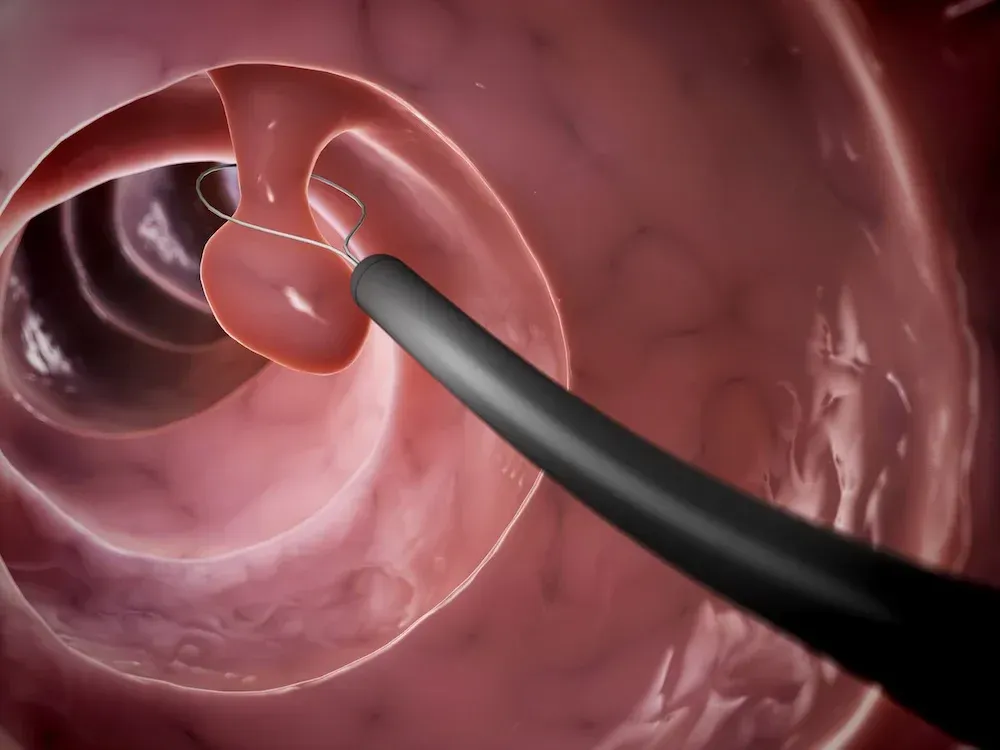
Hemorrhoids, which are swollen veins, may develop internally. Internal hemorrhoids grow inside the lower rectum and can cause bleeding, itching, swelling soiling and other bothersome symptoms. Prolapsed internal hemorrhoids push through the anal opening and may cause pain or irritation.
Hemorrhoids can also grow externally. External hemorrhoids form under the skin around the anus, causing pain, itching and bleeding. It’s possible to have internal and external hemorrhoids at the same time.
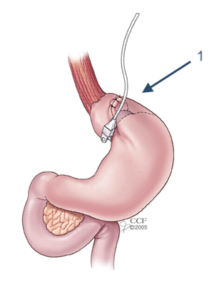
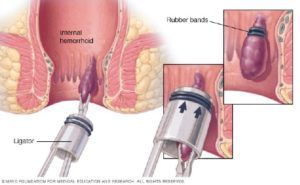
If you’ve tried home remedies or over-the-counter (OTC) creams and have found no relief, hemorrhoid banding treatment might help. Unlike OTC remedies, which only work temporarily, hemorrhoid banding offers a long-term solution. Hemorrhoid banding, also called hemorrhoid ligation, is a non-surgical, painless procedure that a doctor can perform in their office. It’s a straightforward treatment method that involves placing a rubber band around the base of the hemorrhoid. The rubber band prevents blood flow to the hemorrhoid and causes it to wither and eventually fall off on its own.
How Successful Is Hemorrhoid Banding?
In general, the success rate of hemorrhoid banding falls between 70% and 97%, but this depends on the technique used and the hemorrhoid grade. The CRH O’Regan System is a hemorrhoid banding method that’s proven to be 99% effective. This technique is on par with hemorrhoid surgery but features a much lower complication rate.
What Will I Learn in This Guide?
If you’ve tried treating your hemorrhoids at home but have had no success, you may be considering hemorrhoid banding treatment, and you probably have some questions. In this guide, we hope to address your concerns and paint a clearer picture of this minimally invasive hemorrhoid treatment. We’ll answer questions such as:
- How does rubber band ligation work?
- Is hemorrhoid banding painful?
- How long does it take to recover from hemorrhoid ligation treatment?
- Is hemorrhoid banding worth it?
Table of Contents
Chapter 1: What Is Hemorrhoid Banding?
To understand the hemorrhoid banding procedure, it first helps to know how hemorrhoids form. Hemorrhoids can develop any time a person puts too much pressure on the veins in the rectal area. For example, during a bowel movement, the anal tissue fills with blood to aid the process. If you strain during a bowel movement, you may increase pressure in anal veins, causing these veins to swell or stretch. Usually, this swelling resolves quickly after straining, but sometimes the tissue remains engorged. The swollen tissue is called a hemorrhoid.
Other factors that may cause too much pressure to build include:
- Sitting on the toilet too long
- Pregnancy
- Obesity
- Recurring constipation or diarrhea
- Not eating enough fiber
The risk of developing hemorrhoids also increases if you are between 45 and 65 years old. However, hemorrhoids can happen at any age, and it’s not uncommon for young people to experience hemorrhoids. Most people will have a hemorrhoid at some point in their life.
Fortunately, today’s patients do not have to live with the discomfort of having hemorrhoids, nor do they have to choose surgery to find relief.
Hemorrhoid banding, or rubber band ligation, is a painless, minimally invasive method used to treat internal hemorrhoids and relieve external hemorrhoid symptoms.
According to an article published in the World Journal of Gastrointestinal Surgery, rubber band ligation is one of the most commonly used and cost-effective treatments for internal hemorrhoids. In this chapter, we’ll show you how internal hemorrhoid banding works.
The History of Hemorrhoid Banding
Humans have been treating hemorrhoids for thousands of years. Before the invention of rubber band ligation, physicians used a range of methods to relieve hemorrhoid symptoms, including various surgical and ligation techniques. For example, during the fifth century B.C., Hippocrates wrote about a procedure similar to rubber band ligation, which involved tying hemorrhoids with a thick woolen thread “until they drop off.”
It wasn’t until the 1950s that Paul C. Blaisdell first described rubber band ligation as we know it today. The procedure was based on Blaisdell’s idea that internal hemorrhoids are easy to access and have few pain-sensitive nerve endings. Due to the procedure’s simplicity, doctors could use rubber band ligation to provide hemorrhoid treatment in their office rather than in a hospital.
Then, in the 1960s, J. Barron modified outpatient hemorrhoid ligation by using rubber bands and a device called the Barron band ligator. The Barron hemorrhoid ligator is a metal device that uses forceps to grasp the hemorrhoid before placing a rubber band around its base. Since Barron’s technique, various types of forceps have been invented to perform rubber band ligation.
Even though Barron’s ligation method is generally considered simple and safe, it needed improvement. Doctors found that grasping the hemorrhoid with forceps wasn’t always easy and could cause post-procedure pain.
In 1997, laparoscopic surgeon Dr. Patrick J. O’Regan improved hemorrhoid banding instruments by inventing a painless suction device called the CRH O’Regan ligato r. Doctors can use the CRH O’Regan ligator to safely band hemorrhoids within seconds in their own office, and without the patient experiencing any pain.
Today, over a million rubber band ligations have been performed using CRH O’Regan technology.
How Does Hemorrhoid Banding Work?
When a doctor uses a ligator to place a tiny elastic band around a hemorrhoid, it cuts off the hemorrhoidal tissue’s blood supply. This causes the hemorrhoid to painlessly wither and fall from the living tissue in about a week. The surrounding tissue then forms a small scar as it heals. Once a scar forms where the hemorrhoid used to be, it helps keep hemorrhoids from coming back in the same spot.
When Does a Gastroenterologist Recommend Hemorrhoid Banding?
Your gastroenterologist may recommend rubber band ligation to treat hemorrhoids that are prolapsed or causing symptoms such as:
- Pain
- Bleeding
- Itching
- Swelling
- Soiling
Hemorrhoids can become itchier or more painful over time if they remain untreated. Any patient who suffers from recurring hemorrhoid symptoms might consider hemorrhoid banding.
Types of Hemorrhoid Banding
Physicians can use several techniques and specialized tools to perform hemorrhoid banding. For example, ligators feature variations in the grip. Some ligators have a pistol grip, while others feature a scissors grip. The mechanisms for capturing the hemorrhoid and releasing the band also vary.
Even though the following procedures all aim to ligate hemorrhoids, they may produce different results since they involve distinct devices and techniques. Here are the various types of hemorrhoid banding:
Traditional Rubber Band Ligation
During a traditional rubber banding hemorrhoid procedure, the doctor clamps the hemorrhoid with metal forceps and pulls it away from the anal wall. Next, the doctor places a rubber band around the hemorrhoid to cut off blood flow, causing it to dry up and eventually fall off. Traditional rubbing band ligation takes five to 10 minutes, and patients may require up to three days to recover.
This procedure usually causes post-procedure pain and bleeding, and physicians often prescribe pain medication to help patients get through their recovery. According to the World Journal of Gastrointestinal Surgery , pain is one of the most common complications of traditional rubber band ligation and occurs in about 25% to 50% of patients.
The post Hemorrhoid Banding appeared first on Gastro SB.