Home and Office Symptomatic Hemorrhoid Treatment
INTRODUCTION
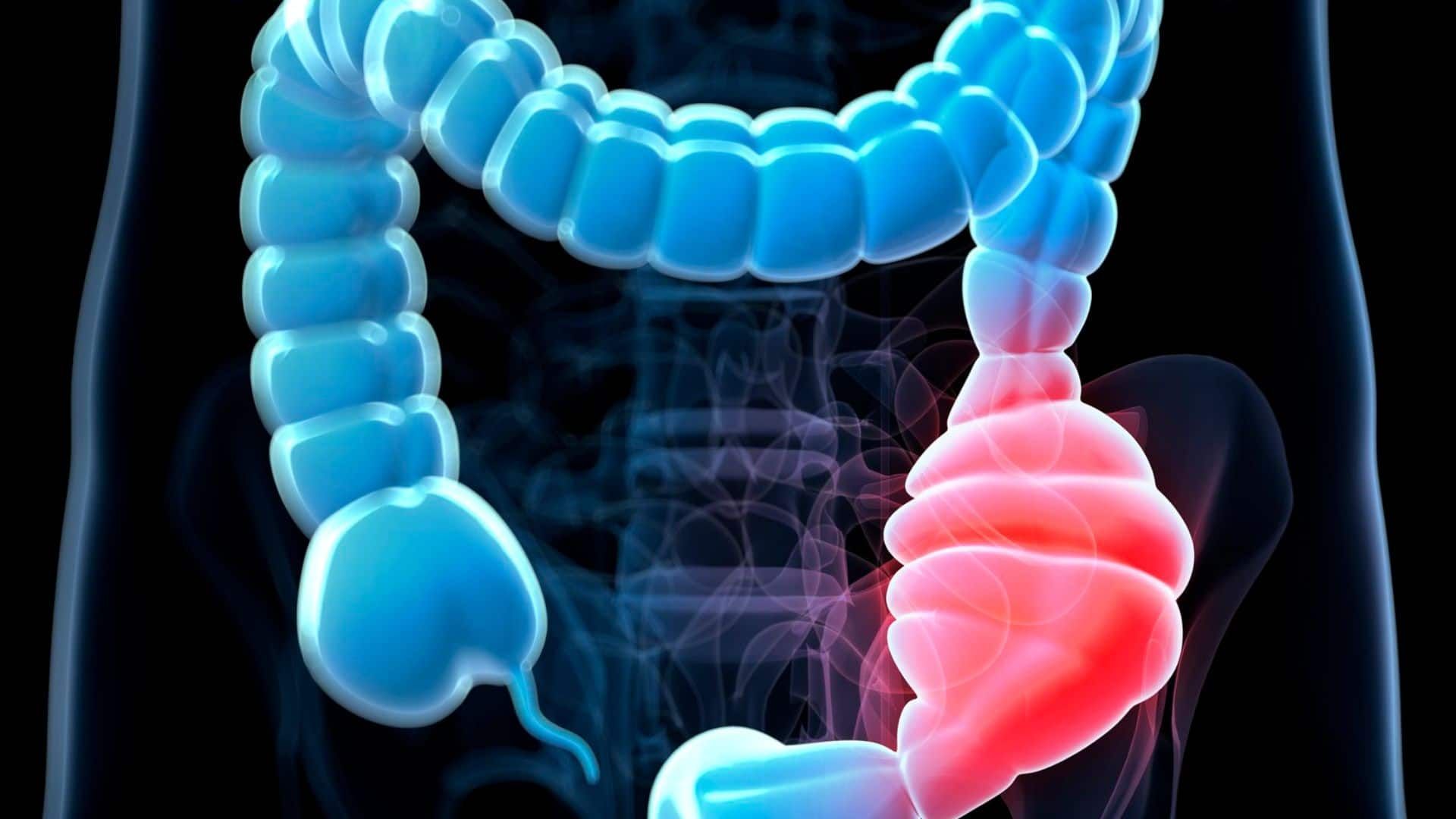
Hemorrhoids are collections of submucosal, fibrovascular, arteriovenous sinusoids that are part of the normal anorectum. In epidemiologic studies conducted in Korea, England, and Austria, between 14 and 39 percent of the population had hemorrhoids; however, many were without symptoms. Without any symptoms, hemorrhoid treatment is not required.
By contrast, an estimated 10 million people in the United States complained of hemorrhoids, corresponding to a prevalence of 4.4 percent. The most common complaint associated with hemorrhoidal disease is painless rectal bleeding during defecation with or without tissue prolapse. Other typical symptoms include anal pruritus or pain and a lump at the anal verge due to thrombosis or strangulation. All are conditions treated by a gastroenterologist.
Those presenting for symptomatic hemorrhoids probably represent a group with relatively severe disease. Because a large variety of over-the-counter products are available and marketed for the treatment of hemorrhoids, patients often self-diagnose and self-treat before seeking medical attention. Incidentally, the quality of information about hemorrhoids on the internet is highly variable, and a significant proportion of websites assessed are poorly informed (40 percent in one study).
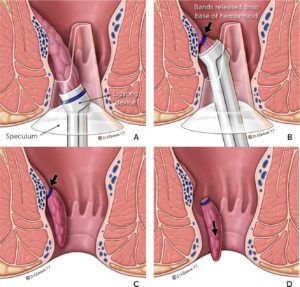
Several options are available for the treatment of symptomatic hemorrhoids, and most patients with low-grade internal hemorrhoids will have relief with home-based conservative treatment or office-based procedures, performed by a gastroenterologist , that are reviewed in this topic. Surgery is indicated for low-grade hemorrhoids that are refractory to home- or office-based treatments, high-grade hemorrhoids, and complicated hemorrhoids. Surgical treatment of hemorrhoids is reviewed separately.
CLASSIFICATION OF HEMORRHOIDS
Hemorrhoids are classified relative to their relationship to the dentate line.
- Internal hemorrhoids are proximal to or above the dentate line. Tissues above the dentate line receive visceral innervation, which is less sensitive to pain and irritation. Thus, internal hemorrhoids are amenable to a variety of office-based procedures that can be carried out with minimal or no anesthesia. Internal hemorrhoids are further subclassified into four grades based on the degree of prolapse from the anal canal.
- External hemorrhoids are distal to or below the dentate line, where tissues are innervated somatically, and therefore are more sensitive to pain and irritation. As a result, symptomatic external hemorrhoids that are refractory to conservative management are generally treated surgically under anesthesia, with the exception of small, acutely thrombosed external hemorrhoids, which can sometimes be treated in the office.
- Mixed internal and external hemorrhoids straddle the dentate line and are generally treated in the same way as are external hemorrhoids.
TREATMENT APPROACHES BY SYMPTOMS
Patients generally complain of hemorrhoids for one of four symptoms:
Irritation or pruritus — Irritation or pruritus from internal or external hemorrhoids (no bleeding or thrombosis) can be treated with a variety of analgesic creams, hydrocortisone suppositories, and warm sitz baths. These treatments, particularly hydrocortisone, should not be used for longer than one week, since side effects may occur, such as contact dermatitis with analgesic creams or mucosal atrophy with steroid creams. If there is no improvement after one week, other nonsteroidal creams can be tried.
Bleeding hemorrhoids — External hemorrhoids generally do not bleed, unless a patient has spontaneously evacuated a thrombosed hemorrhoid; it is usually self-limited. Treatment of bleeding hemorrhoids is initially conservative, such as with dietary modification or external creams. Persistently bleeding internal hemorrhoids can be treated using office-based procedures (eg, rubber band ligation). For external hemorrhoids, the only alternative is surgery since external hemorrhoids are not amenable to banding.
Thrombosed hemorrhoids — Thrombosis is usually associated with pain. Organization and resorption of clot occurs within several days following thrombosis of internal or external hemorrhoids, lessening the degree of pain. Conservative treatment of thrombosed hemorrhoids is usually sufficient. Exceptions include those with severe pain and thrombosed external hemorrhoids and the rare case of concomitant thrombosis of external and internal hemorrhoids (sometimes seen after childbirth). It is important to appreciate that thrombosis of grade III and IV internal hemorrhoids usually persists after the conservative therapies outlined above and may require definitive treatment.
Prolapsed internal hemorrhoids — Internal hemorrhoids are graded from I to IV.
As the grade becomes worse, there is a greater benefit to office-based procedures or surgery. For grade III hemorrhoids, one can first try rubber band ligation, which is often successful after one or two applications. If the rubber band ligation is not effective, then surgery is recommended. For grade IV hemorrhoids, surgery is the best treatment.
CONSERVATIVE TREATMENT FOR ALL PATIENTS
The initial treatment approach to most patients with new-onset symptomatic hemorrhoids is conservative, consisting of dietary/lifestyle modification and topical or oral medications to relieve symptoms. Conservative treatment is successful for most patients and can be continued for as long as the patient wishes.
Dietary and lifestyle modification — There is strong evidence from multiple randomized trials that increased fiber intake improves symptoms of hemorrhoid bleeding and mild prolapse. The other recommendations for dietary and lifestyle modifications are based on common sense rather than data.
- Patients should ingest 20 to 30 g of insoluble fiber per day and drink plenty of water (1.5 to 2 liters per day). Both are necessary to produce regular, soft stools, which reduce straining at defecation. It could take six weeks to fully realize the beneficial effect of fiber.
Many commercially available fiber supplements are available to reduce constipation. Many contain either psyllium or methylcellulose. Neither has been shown to have a particular advantage over the other in treating hemorrhoidal disease. For patients who are unwilling to take fiber supplements, a detailed listing of the fiber content of various foods can be helpful. Because fiber has other salutary effects, is safe to use, and may help to prevent recurrence, we recommend augmentation of fiber in the diet indefinitely.
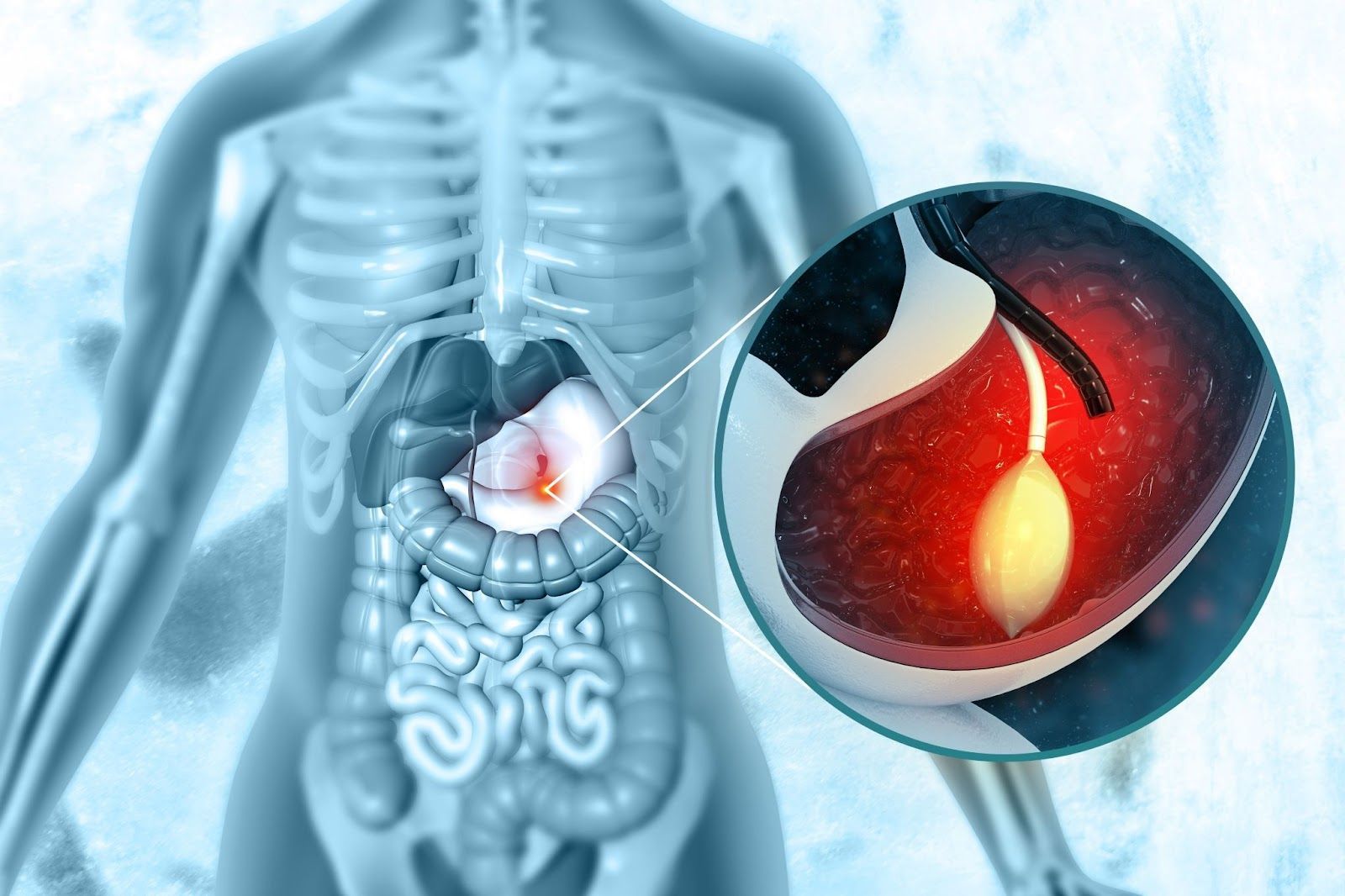
Adding fiber to the diet is beneficial for patients with bleeding.
In an illustrative study, supplementation with psyllium for six weeks was associated with improvement in bleeding compared with untreated controls. In a later trial, 50 patients with bleeding internal hemorrhoids were randomly assigned to receive either a commercially available fiber preparation ( Plantago ovata ) or placebo. Endoscopy was performed before and after treatment. After 15 days of treatment, those who had received fiber supplementation had significantly fewer bleeding episodes and a reduction in the number of hemorrhoids seen on endoscopy.
The benefit of fiber for irritation, pruritus, or prolapse is less well established than for bleeding. Fiber supplementation may relieve pruritus related to fecal soilage since the bulking effect of fiber may reduce leakage of liquid stool. In one study, fiber supplementation had no effect on hemorrhoidal prolapse.
- Patients should refrain from straining or lingering (eg, reading) on the toilet.
- Patients should have regular physical exercise.
- If possible, patients should avoid medications that can cause constipation or diarrhea.
- Patients should also limit their intake of fatty foods and alcohol, which can exacerbate constipation. Although a popular myth, eating spicy food (eg, red hot chili peppers) had no effect on hemorrhoid symptoms such as irritation and pruritus in a controlled study.
Medications for symptomatic relief — Numerous medications, many over-the-counter, are available to treat hemorrhoids. Commonly used medications for hemorrhoids include oral or local analgesics to treat pain, topical agents to reduce local swelling or treat contact dermatitis, therapies to reduce sphincter spasm, and venoactive agents (phlebotonics) to increase venous tone of hemorrhoidal tissues. Each of these may be effective for treating one or more of the symptoms of hemorrhoidal disease (ie, irritation, pruritus, bleeding, thrombosis, pain).
However, data on long-term efficacy or side effects are lacking, with a few exceptions. There is high-quality evidence that phlebotonics (eg, flavonoid, hydroxyethylrutoside, calcium dobesilate) can improve hemorrhoid symptoms such as itch and bleeding. The use of phlebotonics for hemorrhoids is common in Europe and Asia but not North America. Other medical therapies for symptomatic hemorrhoid disease are poorly studied in the medical literature. The choice of these medications is informed more by marketing and patient perception than by actual evidence.
Topical analgesics and steroids — Topical ointments containing anesthetics, steroids, emollients, and antiseptics are often self-prescribed by the patients for quick symptomatic relief. However, there is a lack of strong scientific evidence that supports the use of topical ointments.
Topical analgesics, such as mixed hydrocortisone-lidocaine, are effective for relieving acute pain associated with hemorrhoids. However, topical ointments should not be used for longer than one week, to avoid adverse effects such as contact dermatitis.
Topical steroids, such as hydrocortisone cream or suppository, may shrink the hemorrhoids and relieve the associated pruritus but have not been well evaluated for effectiveness in treating thrombosed hemorrhoids. If they are used, some experts suggest applying cream rather than using suppositories. Steroid cream should be applied twice a day for no more than seven days. Long-term use should be avoided because of potential thinning of perianal and anal mucosa and increasing risk of injury. If symptoms are persistent, an alternative nonsteroidal ointment should be used.
Venoactive agents — Phlebotonics are primarily used in Europe and Asia to treat acutely inflamed and bleeding hemorrhoids. Phlebotonics have not been approved by the US Food and Drug Administration for the indication of hemorrhoids.
Phlebotonics are a heterogenous class of drugs consisting of plant extracts (ie, flavonoids such as hydroxyethylrutoside) and synthetic compounds (eg, calcium dobesilate). Because phlebotonics improve venous tone, microvascular permeability, lymphatic activity, and microcirculatory nutritive flow, they may reduce bleeding associated with hemorrhoids. Some studies have found that hydroxyethylrutoside reduces acute and recurrent hemorrhoidal attacks, including those in pregnant women. In one study, phlebotonics were useful in bridging patients with advanced hemorrhoid disease to surgery. However, many of the studies had important methodological limitations.
Antispasmodic agents — Several types of agents (nitric oxide donors) can be useful for reducing anal sphincter spasm. A small series suggested that topical 0.5% nitroglycerin ointment may provide temporary analgesia by reducing internal anal sphincter spasm. This dose may be associated with side effects such as headache. A lower dose of nitroglycerin has been used in patients with anal fissures.
Sitz baths — Sitz baths are an intuitive topical treatment for acute flare-ups of hemorrhoids to reduce inflammation and edema and relax the sphincter muscles. Patients with significant hemorrhoid disease tend to have elevated sphincter tone. Manometric studies have confirmed that application of moist heat to the perianal area can lower the internal sphincter and anal canal pressures. Sitz baths can relieve irritation and pruritus as well as spasm of the anal sphincter muscles. They should be used with warm, rather than cold, water two to three times per day. A commercially available portable bowl allows for use at the workplace.
Source: Update ®
The post Home and Office Symptomatic Hemorrhoid Treatment appeared first on Gastro SB.