Patient Education: Procedures for Weight Loss & Surgery (Beyond the Basics)

WEIGHT LOSS OVERVIEW
Bariatric surgery (from the Greek words “baros,” meaning “weight,” and “iatrikos,” meaning “medicine”) is the term for a surgery that is done to help you lose weight. Bariatric surgery is not recommended for everyone who is overweight or obese. However, it may be an option if you are obese and have not been able to lose weight with other procedures for weight loss , or if you have other medical conditions that are related to being obese like high blood pressure, high cholesterol, arthritic joint diseases, and diabetes.
Body mass index (BMI) is a way to measure body fat that is based on your height and weight. A person is categorized as underweight, healthy weight, overweight (BMI of 25 to 29.9), or obese (BMI of ≥30) based on his or her BMI. While not every person with a high BMI is unhealthy, the use of BMI to identify unhealthy patients is a very important screening tool.
SHOULD I HAVE SURGERY TO LOSE WEIGHT?
Weight loss surgery is recommended ONLY for people with one of the following
- Severe obesity (body mass index [BMI] above 40).
- BMI above 35 with a serious medical problem related to obesity (including diabetes, severe joint pain, sleep apnea, and many others) that would improve with weight loss.
- BMI above 30 with specific conditions, including a certain type of diabetes or a combination of diseases like high blood pressure, sleep apnea, high cholesterol, and diabetes (also known as “metabolic syndrome”).
- Certain races, such as Southeastern Asians and Indians, have more truncal obesity and will experience the effects of obesity at lower BMIs; consequently, these patients may be eligible for consideration of surgery at a lower BMI of 27.5 kg/m 2 . This may apply to patients who have immigrated to the United States but may not apply to their future generations.
Different surgeons, weight loss clinics , weight loss programs, and insurance companies have different requirements around making healthy lifestyle changes (ie, healthy sleep habits , nutrition, and activity habits) before offering surgery. Occasionally, a person may have enough success losing weight through these lifestyle changes that he or she decides not to go through with a bariatric procedure. In other cases, a person may manage to reduce his or her BMI to the point where it falls below the required minimum for surgery. Many surgeons will still proceed with weight loss surgery in these situations, since the person met the requirements when he or she started the program. Since obesity is considered a chronic disease, the American Society for Metabolic and Bariatric Surgery supports proceeding with surgery in these situations because of the high likelihood that the weight will return. However, it’s important to talk to your surgeon about his or her policies and requirements. Insurance coverage for weight loss surgery also varies by carrier and policy, so be sure you understand your benefits and options.
You should also be sure that you understand the potential risks and benefits of weight loss surgery. You must be motivated and willing to make lifelong changes in how you eat and live to reach and maintain a healthier weight after surgery. You must also be realistic about the amount of weight loss you can expect after surgery.
PREPARING FOR SURGERY
Most people who have weight loss surgery will meet with several specialists before surgery is scheduled. This often includes a gastroenterologist , a dietitian, a mental health counselor, a doctor who specializes in care of obese people, and a surgeon who performs weight loss surgery (bariatric surgeon). You may need to work with these providers for several weeks or months before surgery.
- The nutritionist will explain what and how much you will be able to eat after surgery. A good nutritionist can also give you information about how to prepare foods and read food labels to help you keep track of your caloric intake. The nutritionist will also give you a nutrition plan for after surgery to help maintain weight loss.
- The mental health specialist will help you to cope with stress and other factors that can make it harder to lose weight or trigger you to eat. He or she can also help you make behavioral changes that may lead to a healthier lifestyle.
- The medical doctor will determine whether you need other tests, counseling, or treatment before surgery. He or she might also help you begin a medical weight loss program so that you can lose some weight before surgery.
- The bariatric surgeon will meet with you to discuss the surgeries available to treat obesity and the pros and cons of each type of surgery. He or she will also make sure you are a good operative candidate.
- Starting a serious and regular exercise program prior to surgery will help you prepare mentally and physically for surgery, help you reduce weight prior to surgery, and allow you to have a program you might continue after you recover.
TYPES OF SURGERY FOR WEIGHT LOSS
There are several types of weight loss surgeries, the most common being gastric bypass, gastric sleeve, and gastric balloon. You and your surgeon will work together to decide which surgery, if any, is right for you.
Gastric bypass — Roux-en-Y gastric bypass (RYGB), also called gastric bypass, helps you to lose weight by reducing the amount of food you can eat and reducing the number of calories and nutrients you absorb from the food you eat.
To perform gastric bypass, a surgeon creates a small stomach pouch by dividing the stomach and attaching it to the small intestine. This helps you to lose weight in two ways:
- The smaller stomach can hold less food than before surgery. This causes you to feel full after eating a very small amount of food or liquid. Over time, the pouch might stretch, allowing you to eat more food.
- The body absorbs fewer calories, since food bypasses most of the stomach as well as the upper small intestine. This new arrangement seems to decrease your appetite and change how you break down foods by changing the release of various hormones.
Gastric bypass can be performed as an open surgery (through an incision on the abdomen), but the majority of cases are done laparoscopically, which uses smaller incisions and longer instruments. Both the laparoscopic and open techniques have risks and benefits.
Gastric bypass has a high success rate, and people lose an average of 70 to 75 percent of their excess body weight in the first year. For a person who is 120 pounds overweight, an average of 85 to 90 pounds of weight loss would be expected. Weight loss typically levels off after one to two years, with an overall excess weight loss between 60 and 70 percent after five years.
Gastric sleeve — Gastric sleeve , also known as sleeve gastrectomy, is a surgery that reduces the size of the stomach and makes it into a narrow tube. The new stomach is much smaller, does not stretch when eating, and produces less of the hormone (ghrelin) that causes hunger, helping you feel satisfied with less food.
Sleeve gastrectomy is considered less aggressive than gastric bypass because the intestines are not rearranged, and there is less chance of malnutrition. It also does not require any permanently implanted device.
The gastric sleeve has a good success rate, and people lose an average of 60 to 65 percent of their excess body weight at two years after their procedure. For a person who is 120 pounds overweight, this would mean losing about 72 to 78 pounds. As with gastric bypass, it is important to follow an appropriate lifestyle after surgery. The long-term success is more varied than the gastric bypass.
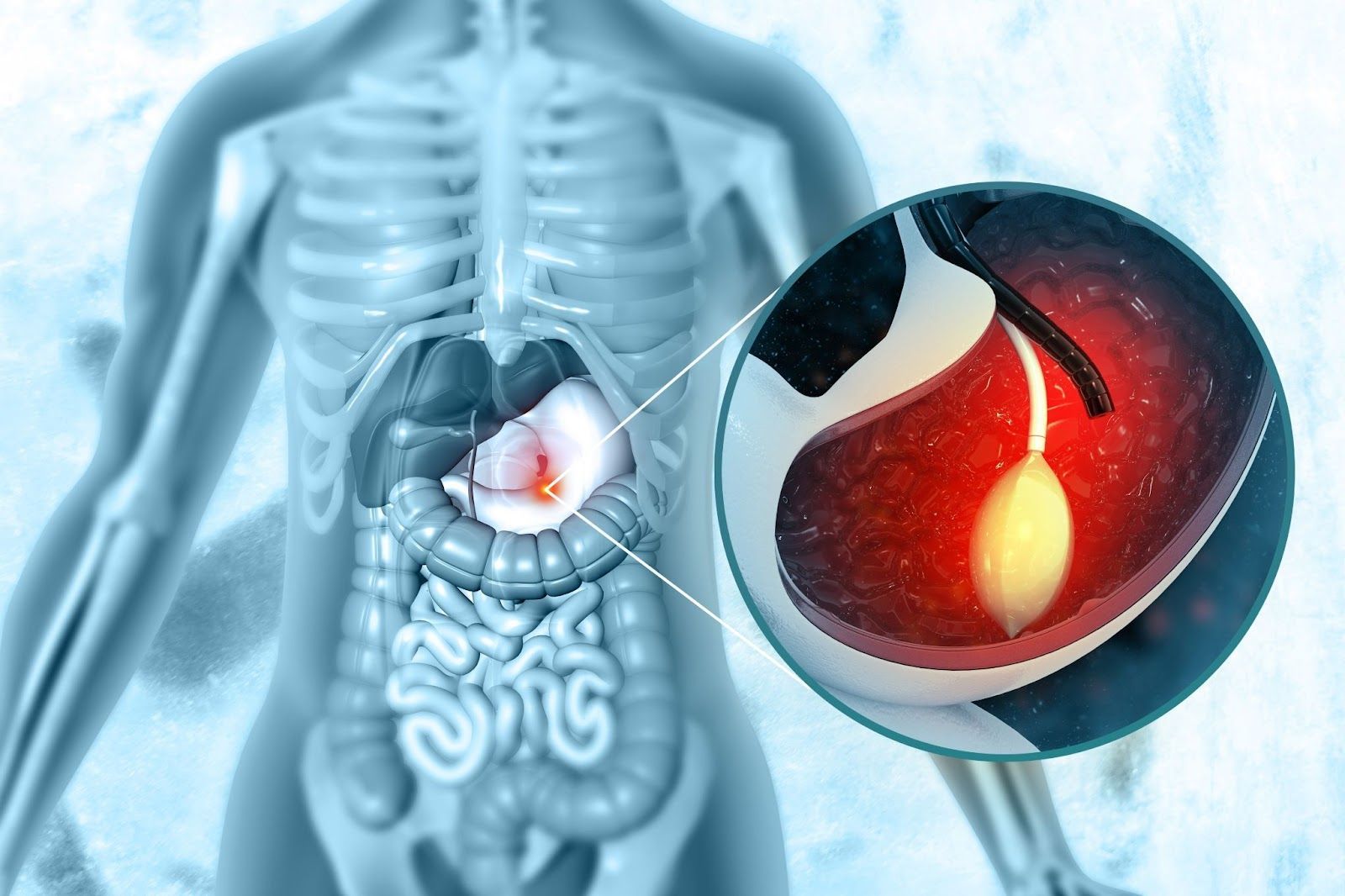
Gastric balloon — The gastric balloon is a procedure whereby an inflatable balloon is placed inside your stomach via your mouth and esophagus using an endoscope. It also works by restricting the amount of food you can eat at one time.
Balloon placement still requires anesthesia, but it does not require an incision. The balloon is meant to be placed for up to six months, and removal usually requires a second procedure. This is an increasingly popular choice because it is relatively safe, easy to perform, and does not require any anatomical changes. The weight loss at six months is about 25 to 38 percent of your excess weight. After the balloon is removed, some, but not all, patients are able to maintain the weight loss.
The use of gastric balloon for weight loss is endorsed by the American Society for Metabolic and Bariatric Surgery. There are several commercially available balloons on the United States market.
Other procedures — Other procedures that are gaining popularity include the duodenal switch (DS), the mini-gastric bypass (MGB), and the single-anastomosis duodenal ileal bypass (SADI). These less common procedures work similarly to the gastric bypass in that they restrict intake and absorption of the food you eat.
The DS is endorsed by the American Society for Metabolic and Bariatric Surgery for certain people, while the MGB and SADI are becoming more accepted as reliable procedures. Not every bariatric surgeon does all of these less common procedures, some of which are associated with different risks than the more common procedures.
In addition to bariatric surgery, other procedures are being investigated to induce weight loss but should be considered as experimental or of limited efficacy:
- One procedure is called “vagal blockade” and involves implanting a device in the abdomen. The device blocks the nerve signals between the brain and the stomach, reducing feelings of hunger.
- A procedure called the “AspireAssist” involves placing a tube into your stomach through the abdominal wall. After eating, you use the tube to suction out part of the stomach contents to reduce caloric intake.
Although these procedures have been approved by the US Food and Drug Administration (FDA), the FDA approvals only certify that they are safe, not necessarily that they are effective. These investigational procedures are not as effective as surgery and may not be appropriate for everyone. If you are obese or overweight and having trouble losing weight through lifestyle modification alone, talk to your doctor about what options might be available for you.
Adjustable gastric banding (AGB), or “lap banding,” is a surgery that involves placing a band around the opening to the stomach. This reduces the amount of food that you can eat at one time; the band can be adjusted to be tighter (further restricting the amount of food the stomach can hold) or looser (allowing you to eat more). AGB is no longer done because it is associated with a higher rate of failure (and need for reoperation) as compared with other procedures.
COMPLICATIONS OF SURGERY FOR WEIGHT LOSS
A variety of complications can occur with weight loss surgery. The risks of surgery depend upon which surgery you have and any medical problems you had before surgery. Some of the more common early surgical complications (one to six weeks after surgery) include:
- Bleeding
- Infection
- Blockage or leaks in the bowels
- Dehydration, nausea, and vomiting
Important medical complications after surgery can include blood clots in the legs or lungs, heart attack, pneumonia, and urinary tract infection. Although deaths have been reported after all major procedures, including gastric balloon, they are very unlikely to happen.
Complications may happen in any setting, and, if they do, they may be best managed at centers experienced in weight loss surgery. In general, centers with experience in weight loss surgery have:
- Board-certified doctors and surgeons with either specific training in, or who have performed a large volume of, bariatric surgery.
- A reliable method of communication to reach your providers at all hours, including after hours and on holidays.
- A team of support staff (dietitians, counselors, nurses).
- Long-term follow-up after surgery.
- Hospital staff experienced with the care of weight loss patients. This includes nurses who are trained in the care of patients immediately after surgery and anesthesiologists who are experienced in caring for the morbidly obese.
EFFECTIVENESS OF SURGERY FOR WEIGHT LOSS
The goal of weight loss surgery is to reduce the risk of illness or death associated with obesity. Weight loss surgery can also help you to feel and look better, reduce the amount of money you spend on medicines, and cut down on sick days from work.
As an example, weight loss surgery can improve health problems related to obesity (diabetes, high blood pressure, high cholesterol, sleep apnea, and many others) to the point that you need less or no medicine.
Finally, weight loss surgery might reduce your risk of developing heart disease, cancer, and certain infections.
AFTER WEIGHT LOSS SURGERY
You will need to stay in the hospital until your team feels that it is safe for you to leave (on average, one to three days). Do not drive if you are taking prescription pain medicine. Begin exercising as soon as possible once you have healed; most weight loss centers will help design an exercise program for you.
Once you are home, it is important to eat and drink exactly what your doctor and dietitian recommend. You will see your doctor, nurse, and dietitian on a regular basis after surgery to monitor your health, diet, and weight loss.
You will be able to slowly increase how much you eat over time, although it will always be important to:
- Continuously reassess intake and ensure that you are maintaining healthy habits because weight regain is always possible
- Choose healthy foods and do not skip meals
- Chew your food slowly and completely
- Avoid eating while “distracted” (such as eating while watching TV)
- Stop eating when you feel full
- Drink liquids at least 30 minutes before or after eating
- Be aware of the calories you ingest daily
- Avoid foods high in fat or sugar
- Take vitamin supplements, as recommended
- Make exercise part of your daily routine
- Ensure that you are getting at least eight hours of sleep per night
It can take several months to learn to listen to your body so that you know when you are hungry and when you are full. You may dislike foods you previously loved, and you may begin to prefer new foods. This can be a frustrating process for some people, so talk to your dietitian if you are having trouble.
It usually takes between one and two years to lose weight after surgery. After reaching their goal weight, some people have plastic surgery (called “body contouring”) to remove excess skin from the body, particularly in the abdominal area.
Before you decide to have weight loss surgery, you must commit to staying healthy for life. This includes following up with your healthcare team, exercising most days of the week, and eating a sensible diet every day. It can be difficult to develop new eating and exercise habits after weight loss surgery, and you will have to work hard to stick to your goals. You need to remember that surgery is only a tool of weight loss that will only work if it is used properly.
Recovering from surgery and losing weight can be stressful and emotional, and it is important to have the support of family and friends. Working with a social worker, therapist, or support group can help you through the ups and downs.
Source: Uptodate ®
Learn More About Weight Loss Procedures
Patient Education: Procedures for Weight Loss (The Basics)
Procedures for Weight Loss . . . WE’RE IN IT TOGETHER
Obesity in Adults: Behavioral Therapy & Weight Loss Clinics
Patient Education: Health Risks of Obesity & Weight Loss Tips (The Basics)
Gastro SB Weight Loss Clinic: Medications Used for Weight Loss
Weight Loss Tips and Medications
Patient Education: Health Risks Of Obesity
Medications Used For Weight Loss
Procedures For Weight Loss Treatments
Obesity In Adults Dietary Therapy And Weight Loss Coaches
The post Patient Education: Procedures for Weight Loss & Surgery (Beyond the Basics) appeared first on Gastro SB.