Bariatric Procedures for Weight Loss and the Management of Severe Obesity
INTRODUCTION
Procedures for weight loss include a combination of volume-restrictive, intestinal hormone alteration, and nutrient-malabsorptive procedures that affect satiety, absorption, and insulin sensitivity in conjunction with behavior modification to achieve and sustain weight loss.
A consultation with a multidisciplinary bariatric team, including a gastroenterologist , provides extensive education on nutrition, good psychological responses, and lifestyle modification needed for a patient to be successful with a surgical weight loss procedure. Proper bariatric care also includes lifelong surveillance. A reliable bariatric program will provide a comprehensive information session for potential surgical candidates that will detail realistic outcomes from weight loss surgery, including morbidities and mortalities.
This topic will review the contemporary, investigational, revisional, and obsolete bariatric procedures offered to patients with a surgical indication. The indications are a body mass index (BMI) of greater than or equal to 40 kg/m 2 , a BMI of 35 to 39.9 kg/m 2 with an obesity-related comorbidity (eg, diabetes, hypertension, gastroesophageal reflux disease, osteoarthritis, among many others), or a BMI of >30 kg/m 2 with difficult-to-control type II diabetes mellitus or dysmetabolic syndrome X.
Indications, preoperative preparation, postoperative management, complications, and outcomes of bariatric surgical procedures are described in the following topics:
PREVALENCE
Bariatric surgery is one of the fastest-growing operative procedures performed worldwide, with an estimated >579,000 operations performed in 2014 [ 2 ]. In the United States, close to two million patients underwent bariatric surgery between 1993 and 2016, during which time the field has evolved from exclusively open surgery (gastric bypass or vertical banded gastroplasty) to 98 percent laparoscopic surgery ( gastric sleeve or gastric bypass). Complication and mortality rates have decreased from 11.7 and 1 percent in 1998 to 1.4 and 0.04 percent in 2016. Despite that, only 0.5 percent of eligible patients actually underwent bariatric surgery in 2016 (compared with 0.07 percent in 1993 and 0.62 percent in 2004).
This low percentage of utilization is likely the result of many factors. The increase in the number of patients who need bariatric surgery has likely outpaced the increase in the volume of bariatric surgeries performed. Some patients can be managed without surgery, while others are not suitable surgical candidates because of behavioral or psychosocial issues. There continues to be referral bias from clinicians who still believe either that obesity is a behavior problem rather than a disease for which surgery can be therapeutic, or that bariatric surgery is too risky. Finally, there remains payer resistance to covering bariatric surgery despite its well-documented cost effectiveness.
OVERALL MECHANISM OF WEIGHT LOSS
Bariatric surgical procedures affect weight loss through three fundamental mechanisms: malabsorption, restriction, and the neurohormonal response that regulates hunger and energy balance. Some procedures have both a restrictive and malabsorptive component.
Restriction — Restrictive procedures limit caloric intake by reducing the stomach’s reservoir capacity via resection, bypass, or creation of a proximal gastric outlet. Vertical banded gastroplasty (VBG) and laparoscopic adjustable gastric banding (LAGB) are purely restrictive procedures and share similar anatomical configurations. Both limit solid food intake by restriction of stomach size as the only mechanism of action, leaving the absorptive function of the small intestine intact. These procedures have largely been abandoned. The sleeve gastrectomy has become the main restrictive procedure, but it is probably more successful due to its hormonal effects on hunger control. Procedures such as intragastric balloon placement or aspiration therapy also work by restricting food intake but produce more gradual and modest weight loss with higher recidivism rates compared with other contemporary surgical procedures.
Malabsorption — Malabsorptive procedures decrease the effectiveness of nutrient absorption by shortening the absorption length of the functional small intestine, either through bypass of the small bowel absorptive surface area or diversion of the biliopancreatic secretions that facilitate absorption. Jejunoileal bypass (JIB) and the biliopancreatic diversion (BPD) are examples of malabsorptive procedures. Profound weight loss can be achieved by a malabsorptive operation, depending upon the effective length of the functional small bowel segment. However, the benefit of superior weight loss can be offset by significant metabolic complications, such as protein calorie malnutrition and various micronutrient deficiencies.
Combination of restriction and malabsorption — Established procedures such as the Roux-en-Y gastric bypass (RYGB), the BPD with duodenal switch (BPD/DS), and the single-anastomosis duodenal ileal bypass with sleeve gastrectomy (SADI-S) are both restrictive and malabsorptive. In the RYGB, a small gastric pouch limits oral intake. However, the small bowel reconfiguration provides additional mechanisms favoring weight loss, including dumping physiology, positive hormonal changes, and mild malabsorption. There is an effect on hunger as well, likely due to the hormonal changes.
Less common procedures, including the one-anastomosis gastric bypass (OAGB) and the single-anastomosis duodenal ileal bypass (SADI), also work by restriction and malabsorption as well as hormonal modulation.
PROCEDURES ENDORSED BY THE ASMBS
The American Society of Metabolic and Bariatric surgery (ASMBS) publishes and maintains a list of bariatric procedures that it endorses on its website. Centers accredited by the American College of Surgeons Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) may perform the following procedures without institutional review board (IRB) approval.
Roux-en-Y gastric bypass — The Roux-en-Y gastric bypass (RYGB) remains one of the most commonly performed bariatric procedures. Global trends show an overall decline from approximately 65 percent in 2003 to 47 percent in 2011 of all bariatric procedures performed.
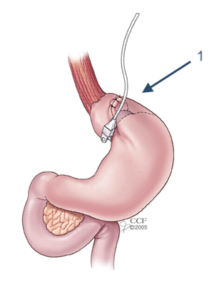
Description of RYGB — The RYGB is characterized by a small (less than 30 mL) proximal gastric pouch that is divided and separated from the distal stomach and anastomosed to a Roux limb of small bowel that is 75 to 150 cm in length. The small gastric pouch and the narrow anastomotic outlet serve to restrict caloric intake, while the major digestion and absorption of nutrients occurs in the common channel where gastric acid, pepsin, intrinsic factor, pancreatic enzymes, and bile mix with ingested food .
The small intestine is divided at a distance of 50 to 150 cm distal to the ligament of Treitz. By dividing the bowel, the surgeon creates a proximal biliopancreatic limb that transports the secretions from the gastric remnant, liver, and pancreas. The Roux limb (or alimentary limb) is anastomosed to the new gastric pouch and functions to drain consumed food. The cut end of the biliopancreatic limb and the Roux limb are then connected 75 to 150 cm distally from the gastrojejunostomy. Major digestion and absorption of nutrients then occurs in the resultant common channel where pancreatic enzymes and bile mix with ingested food. The ideal Roux limb, biliopancreatic limb, and common channel length have not been determined.
Weight loss mechanism of RYGB — While the RYGB, with its small pouch, is primarily a restrictive operation, a malabsorptive component also contributes to weight loss. RYGB has been shown repeatedly to be better than purely restrictive procedures in long-term weight reduction. Gut hormones also have a role in the weight loss seen following gastric bypass.
- Gastrojejunostomy anatomy (connection between the stomach pouch and jejunum) is associated with dumping physiology and causes unpleasant symptoms of lightheadedness, nausea, diaphoresis and/or abdominal pain, and diarrhea when a high-sugar meal is ingested. This response may serve as a negative conditioning response against consumption of a high-sugar diet postoperatively.
- The optimal length of the Roux limb in achieving the best balance between weight reduction and complications of malabsorption is controversial. Increasing Roux limb length can lead to increased malabsorption, since lengthening the Roux limb effectively shortens the common channel limb where major digestion and absorption of the ingested nutrients occurs. At present, most surgeons do not make the Roux length longer than 150 cm. “Distalization” to make a longer biliopancreatic limb length with a shorter common channel has been used to treat patients with inadequate weight loss following standard RYGB, but the risk for metabolic complications increases similar to other malabsorptive operations, and weight loss results vary. It may, in fact, be the length of the biliopancreatic limb that determines the best results for weight loss without malabsorption complications.
- Ghrelin is a peptide hormone secreted in the foregut (stomach and duodenum) that stimulates the early phase of meal consumption. The normal pulsatile release of this orexigenic (appetite-producing) hormone appears to be inhibited in gastric bypass patients due to its unique foregut bypass configuration. Such inhibition of ghrelin has also been observed in laparoscopic sleeve gastrectomy. The reduced ghrelin levels may contribute to the characteristic loss of appetite seen in post-RYGB patients. An exaggerated response of peptide YY (PYY) may also contribute to the loss of appetite. Reduced ghrelin levels may eventually increase to their normal levels.
- Hormones such as glucagon-like peptide-1 (GLP-1) and cholecystokinin (CCK), which are increased after RYGB, may promote an anorectic state.
Expected weight loss from RYGB — The expected loss of excess weight after two years is approximately 70 percent.
The techniques of laparoscopic RYGB are covered in more detail in their own topic.
Sleeve gastrectomy — Sleeve gastrectomy (SG) is a partial gastrectomy in which the majority of the greater curvature of the stomach is removed and a tubular stomach is created. SG was initially offered to patients with super severe obesity (body mass index [BMI] >60 kg/m 2 ) as the first stage in surgical management. The SG is technically easier to perform and viewed as “not as drastic” by patients. In 2016, it was the most commonly performed bariatric procedure in the world and in the United States.
Description of SG — SG is technically easier to perform than the RYGB as it does not require multiple anastomoses. It is also safer as it reduces the risks of internal herniation and protein and mineral malabsorption. The antrum is divided approximately 2 to 6 cm away from the pylorus, and a sleeve is created around a 32 to 40 French bougie. The tubular stomach is small in its capacity (restriction), resistant to stretching due to the absence of the fundus, and has few remaining ghrelin-producing cells. Although SG is a restrictive procedure, gastric motility changes also occur with surgery and may affect weight loss outcomes. The SG will make the stomach a high-pressure organ with a sphincter at both ends. This is why leaks are more frequent than in RYGBs, and they are more difficult to manage. Additionally, the SG has a much higher incidence of gastroesophageal reflux disease because of its higher-pressure nature.
The laparoscopic approach to an SG can be found at the following link to the SAGES video library’s page on sleeve gastrectomy for morbid obesity.
Weight loss mechanism of SG — SG should not be considered as only a restrictive option for the treatment of severe obesity. It is now a single-stage primary operation, rather than just a bridge procedure to a more technically challenging gastric bypass, biliopancreatic diversion, or SADI-S in high-risk patients. Moreover, the hormonal changes it causes indicate that its success is not only due to restricted food intake. Ghrelin levels decrease and GLP-1 and PYY levels increase, promoting less hunger, while insulin resistance improves and aids glycemic control.
Expected weight loss from SG — At two years, the expected excess weight loss is approximately 60 percent.
The techniques of laparoscopic SG are covered in more detail in its own topic.
Biliopancreatic diversion with duodenal switch — The biliopancreatic diversion with duodenal switch (BPD/DS) is a variant of the biliopancreatic diversion (BPD) In the United States, the role of BPD/DS is not clear. Some surgeons perform this procedure for patients with BMI >50 kg/m 2 , while others reserve it as a revisional procedure for failure to lose weight or weight recidivism after other procedures. BPD results in fat and starch malabsorption. Its use has been limited by the high rates of protein malnutrition, anemia, diarrhea, and stomal ulceration. Because BPD/DS is a technically difficult operation with a high complication rate, it has not been fully embraced as a bariatric procedure.
Description of BPD/DS — The original BPD procedure involves dividing the duodenum from the pylorus, removing the pylorus, and dividing the ileum. The distal ileum is then anastomosed to the stomach and the proximal ileum, with the output from the liver, pancreas, and duodenum (or biliopancreatic limb) anastomosed to the terminal ileum some 50 to 100 cm away from the ileocecal valve. The BPD with a DS procedure involves creating a sleeve gastrectomy with preservation of the pylorus and creation of a Roux limb with a short common channel. The BPD/DS procedure differs from the BPD in the portion of the stomach that is removed, as well as in the preservation of the pylorus, similar to an SG. This allows more forward flow of the contents of the biliopancreatic limb and avoids the complications of stasis that plagued the jejunoileal bypass (JIB). It is associated with a lower incidence of stomal ulceration and diarrhea than with BPD alone. SG complications can still occur with this procedure, though. Although complex, BPD/DS can be performed laparoscopically by experienced surgeons.
Weight loss mechanism of BPD/DS — BPD/DS is a combination of restrictive and malabsorptive weight loss mechanisms. Though less studied than the hormone responses for the SG and RYGB, there is most likely some contribution of altered hormone production to sustained weight loss. For example, ghrelin appears to be suppressed after a BPD/DS. The contribution of gut hormones to weight loss and insulin sensitivity with a BPD/DS is largely unknown.
Expected excess weight loss from BPD/DS — At two years, the expected excess weight loss is approximately 70 to 80 percent.
Single-anastomosis duodenoileal bypass with sleeve gastrectomy — Single-anastomosis duodenoileal bypass with sleeve gastrectomy (SADI-S) is fundamentally a variant of the BPD/DS operation, in which the transected duodenum is anastomosed to a loop of distal small bowel as opposed to the Roux-en-Y configuration used in classic BPD/DS. Thus, there is only one anastomosis. The SADI-S procedure was developed in part to reduce the complexity and therefore the risks of performing a Roux-en-Y configuration with small-diameter distal bowel and a need for two anastomoses.
SADI-S has been endorsed by the American Society for Metabolic and Bariatric Surgery as an appropriate primary metabolic bariatric procedure. Additionally, it has been used as a conversional procedure for inadequate weight loss after either RYGB or SG.
Description of SADI-S — The sleeve is created first, and the duodenum is divided about 4 cm from the pylorus. A single anastomosis is then created between the side of the distal small bowel and the end of the sleeve-like gastric pouch/duodenum.
Most contemporary publications on SADI-S use a common channel length of no less than 300 cm, but SG sizes vary widely, from 34 to 54 Fr.
Weight loss mechanism of SADI-S — The weight loss occurs due to restrictive, malabsorptive, and probably hormonal mechanisms.
Expected excess weight loss from SADI-S — Reports are varied depending on the sleeve size, common channel length, and duration of follow-up, but one meta-analysis of 12 studies shows excess weight loss to be around 85 percent two years after the surgery.
In nonrandomized comparative studies, SADI-S achieved similar percent excess weight losses compared with RYGB, SG, and BPD/DS, but SADI-S patients had fewer anastomotic complications, bowel obstructions, internal hernias, and volvulus, presumably because SADI-S required one fewer anastomosis than the other two procedures. SADI-S, however, was associated with greater risk of chronic diarrhea, even with a 300 cm common channel. With a common channel length less than 300 cm, the rates of malnutrition were very high. It is not clear why a BPD/DS can have a common channel of 150 to 200 cm but the SADI-S does better with a 300 cm common channel.
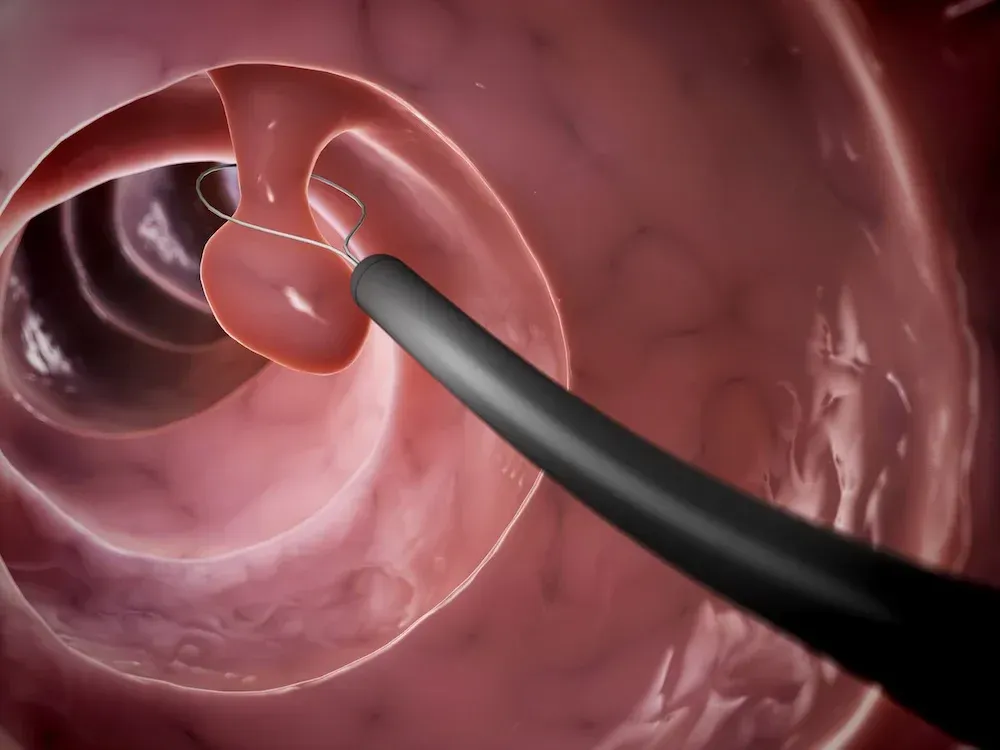
Intragastric balloon — The intragastric balloon (IGB) consists of a soft, saline-filled balloon that promotes a feeling of satiety and restriction. An IGB has been advocated for use as a bridge to a more definitive surgical procedure. Use of the balloon is also approved for patients with class I obesity (BMI 30 to 34.9 kg/m 2 ). Three IGB devices, Orbera, Obalon, and ReShape balloons, have been approved by the US Food and Drug Administration (FDA) to treat obesity in adults with a BMI of 30 to 40 kg/m 2 with one or more comorbid conditions such as diabetes, hypertension, or hypercholesterolemia. They are intended for patients who have failed previous attempts at weight loss through diet and exercise alone.
Other IGB systems are commercially available in various regions and countries but have not received FDA approval in the United States, including one that does not require endoscopic placement or retrieval. Balloon placement is contraindicated in patients who have had previous gastric surgery or who have large hiatal hernias (>5 cm).
Description of IGB — An IGB is typically inserted endoscopically and filled with 400 to 700 mL of saline, generally for a maximum of six months, beyond which time the leak rate increases significantly. A deflated balloon can migrate into the small intestine and cause bowel obstruction. Removal requires a second endoscopic procedure.
Adverse events include nausea, vomiting, reflux, balloon migration, balloon intolerance, balloon leak, and intestinal or stomach perforation. Balloons are typically filled with blue-dyed saline. If the patient’s urine turns blue or green, then a balloon leak should be suspected. Patients should seek immediate medical attention as the balloon would then be at risk for migrating and causing an intestinal obstruction. The ReShape is a two-balloon device so that if one breaks, the second balloon can prevent migration.
Weight loss mechanism of IGB — The IGB is purely a restrictive procedure. Weight loss is dependent on adherence to lifestyle changes and patient compliance.
Expected weight loss from IGB — In one trial, those who were randomly assigned to the ReShape group lost more weight than the control group who received endoscopy without balloon insertion (6.5 kg [6.8 percent of total body weight] versus 3.3 kg [3.3 percent]). Six months after removal of the device, patients kept off 70 percent of their initial weight loss. After two years, patients treated with the ReShape device had significantly greater excess weight loss than controls (25 versus 11 percent).
As much as 33 percent excess weight loss has been reported in trials conducted outside of the United States with devices not approved by the FDA. After five years of surveillance, however, only 23 percent of patients maintained more than 20 percent of their excess weight loss.
IGB therapy for weight loss is discussed in detail in its own topic. One-anastomosis gastric bypass — The one-anastomosis gastric bypass (OAGB) is a modification of the loop gastric bypass and is technically easier to perform than an RYGB because it requires only one anastomosis. OAGB is a simple and safe procedure and can be easily revised, converted, or reversed.
It is also referred to as the mini-gastric bypass. It was endorsed by the ASMBS as a primary procedure in 2022. Outside of the United States, OAGB is a popular operation with an estimated 10,000 procedures done annually.
Description of OAGB — The OAGB is usually performed laparoscopically and includes the division of the stomach between the antrum and body on the lesser curvature. The stomach is further divided in the cephalad direction to the angle of His. This subsequent pouch is anastomosed to a loop of jejunum as an antecolic and antegastric loop gastrojejunostomy. Although there is no consensus on a standardized length, most studies used a 200 cm biliopancreatic limb distal to the ligament of Treitz.
Weight loss mechanism of OAGB — The OAGB combines restrictive as well as malabsorptive properties for weight loss. Though not extensively studied, there are likely hormonal changes that occur such that insulin sensitivity improves and hunger is abated.
Expected excess weight loss — Weight loss outcomes after OAGB appear to be comparable to those of RYGB, with most series reporting 68.6 to 85 percent excess weight lost (EWL) at ≥5 year follow-up. Studies have generally found either superior or comparable weight loss with OAGB compared with laparoscopic sleeve gastrectomy (LSG). Initial evidence suggests that OAGB is similar to RYGB in its ability to induce remission of type 2 diabetes. One trial reported lower glycated hemoglobin (6.1 versus 7.1 percent) after OAGB than after LSG.
A trial of 261 patients (YOMEGA) found similar excess body mass index loss at two years after OAGB (-87.9 percent) and RYGB (-85.8 percent); HbA1C improved to a greater extent after OAGB than RYGB (-2.3 versus -1.3 percent) in patients with type 2 diabetes. However, OAGB was associated with almost twice as many overall serious complications, and more complications related to malabsorption (eg, nutritional deficiency, diarrhea, steatorrhea), than RYGB. This trial used a biliopancreatic limb of 200 cm, which may have caused the excessive malabsorption. Contemporary studies use a shorter limb of 150 to 180 cm instead.
However, although OAGB has a relatively short operative time, low complication rate, and excellent weight loss outcomes, there is a concern for the high rates of alkaline bile reflux. There does not appear to be an associated risk of malignant degeneration. If the bile reflux becomes severe enough, a conversion to an RYGB is used as a rescue procedure.
PRIMARILY REVISIONAL PROCEDURES
Band revisions — For patients who fail the band or who have complications from it that require removal, there are several conversion options that have been published. The band can be replaced, or it can be converted to a sleeve gastrectomy (SG), a Roux-en-Y gastric bypass (RYGB), or biliopancreatic diversion with duodenal switch (BPD/DS) [ 1 ]. The timing of the revision can be important as the gastric tissue may be inflamed or fibrotic due to the band. As a result, some authors have advocated a staged approach. The band is first removed, and then, after a period of 8 to 12 weeks, the stomach is converted to another bariatric procedure.
RYGB revisions — While most people who experience weight recidivism do so because of a failure to adhere to a healthy lifestyle, there are some anatomical reasons that an RYGB might fail. Over time, the patient may lose the sense of restriction if their gastric pouch enlarges, a fistula occurs between the gastric pouch and the remnant stomach, or the anastomosis between the gastric pouch and the Roux limb enlarges. These conditions may be an indication to surgically recreate the gastric pouch and gastrojejunal anastomosis. There are some preliminary data using endoluminal measures to do so that show promise because they avoid the risk of reoperative bariatric surgery, which has a higher morbidity than de novo operations. There are no long-term studies, however, on the durability of these maneuvers.
The concept of “distalization” or revising the jejunojejunostomy anastomosis to make the biliopancreatic limb longer has gained some traction. For these patients, there are no issues with the gastric pouch, but they have regained a significant amount of weight. The biliopancreatic limb is lengthened without sacrificing too much of the common channel. This has resulted in some positive results for renewed weight loss and comorbidity control.
The indication to operate for weight regain still requires a body mass index (BMI) of >40 kg/m 2 , a BMI >35 kg/m 2 with a comorbid condition, or a BMI of >30 kg/m 2 with dysmetabolic syndrome or difficult-to-control type 2 diabetes mellitus.
The laparoscopic approach to a failed RYGB with biliopancreatic diversion with duodenal switch can be found on the following link to the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) video library’s page on laparoscopic conversion of Roux-en-Y gastric bypass to biliopancreatic diversion with duodenal switch.
Sleeve revisions — One criticism of the SG was the durability of the operation as one theorized that, over time, the SG could expand and patients would lose their restriction. The three-year data suggest that SG is comparable to RYGB in terms of sustained weight loss and diabetes remission. At five years, however, at least one study showed that the durability of SG was not as good as that of RYGB because of weight regain and recurrence of diabetes over time. Additionally, sleeve revisions are done for intractable reflux disease in patients with satisfactory weight loss.
Source: Uptodate ®
The post Bariatric Procedures for Weight Loss and the Management of Severe Obesity appeared first on Gastro SB.